How cardiovascular imaging can proactively pinpoint heart problems — and potentially save lives.
Many patients schedule regular mammograms and colonoscopies to screen for cancer, but don’t think of taking the same approach for the heart. That perspective is changing due to ever more sophisticated screening technologies at RWJBarnabas Health (RWJBH), New Jersey’s largest network of noninvasive, advanced cardiovascular imaging centers.
Cardiovascular screenings can catch heart and vascular conditions in early stages. Left untreated, many conditions progressively worsen. But proactive imaging offers opportunities to correct conditions—including aortic valve stenosis, mitral valve regurgitation, aortic aneurysm or increased risk of heart disease due to prior cancer treatments—before they become life-threatening problems such as a heart attack or heart failure.
At RWJBH, advanced imaging technologies are being combined with integrated medical records and artificial intelligence to identify, monitor and track cardiac performance through annual scans.
This increasingly helps cardiologists predict the need for interventions, determine treatments and, with patients, develop heart health plans.
Imaging technologies can save lives, as indicated by patients who have already benefited from proactive scans like these.
EKG
How it helps: Measuring electrical activity in the heart can find abnormalities that may indicate conditions such as irregular heartbeat, clogged arteries, heart damage, heart failure or a heart attack.
Great catch: RJ. A then-16-year old high school football player, RJ discovered through an EKG (administered by an RWJBH screening program for young athletes) that he had an abnormal extra electrical pathway in his heart that could trigger a rapid heart rate. RWJBH electrophysiologists corrected RJ’s condition with a minimally invasive procedure called catheter ablation—and he played his first varsity game just two weeks later.
Stress Echocardiogram
How it helps: Ultrasound imaging that measures the heart’s size, shape, strength and function can identify problems such as faulty valves, structural abnormalities, heart attack damage and heart failure.
Great catch: Virginia. She seemed at low risk of heart disease, but Virginia Haines noticed that she often became short of breath during activities such as climbing stairs. A stress echocardiogram—administered while exercising on a treadmill—found she had an obstructed coronary artery. A procedure called an angioplasty opened the blockage and staved off a heart attack.
Transesophageal Echocardiogram (TEE)
How it helps: TEE is a type of ultrasound that takes pictures from a position inside a person’s esophagus, close to the heart. Its highly detailed images can help reveal problems such as faulty heart valves.
Great catch: Alex. When his primary care physician heard a heart murmur, Alex Martin went for heart testing. Alex was fit, but a TEE discovered that his heart’s mitral valve was abnormally allowing blood to flow backward. A procedure called mitral valve repair restored Alex’s heart function and installed a durable valve capable of lasting the rest of his life.
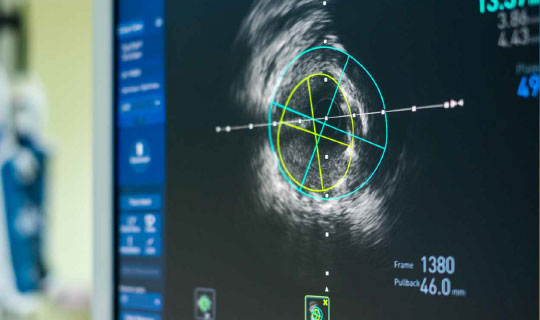
Fractional Flow Reserve CT (FFR-CT)
How it helps: Artificial intelligence helps create a 3-D model of a patient’s cardiac arteries, providing information that helps cardiologists assess blood flow and the significance of any blockages.
Great catch: Ray. As Director of Information Technology and Services at Monmouth Medical Center (MMC) and MMC Southern Campus (MMCSC), Ray Duarte underwent FFR-CT screening during testing of the technology for its pioneering use at MMCSC. The scan unexpectedly discovered that one of his coronary arteries was 99 percent blocked. Undergoing a procedure to open the artery brought Ray back from the brink of a heart attack.
Calcium Score
How it helps: This type of computerized tomography (CT) scan helps cardiologists learn about the presence, location and extent of calcified plaque in coronary arteries that can lead to a heart attack.
Great catch: Tony. Chest discomfort and pain in his left arm prompted Tony to seek help. When preliminary tests were inconclusive, RWJBH cardiologists ordered a calcium score, the most accurate way to detect potentially dangerous plaque buildups. Tony’s high score indicated he was at high risk of a heart attack—which a proactive bypass surgery helped him avoid.
Valve Monitoring
How it helps: Combining technologies such as stress echocardiograms, CT scans and cardiac magnetic resonance imaging (MRI) lets cardiologists track heart valve anatomy, function and physiology. This helps them monitor abnormalities such as buildups of amyloid proteins that can lead to aortic stenosis and heart failure.
Great catch: Helen. A heart murmur provided the first indication that avid walker Helen Blumenthal had a thick, stiff aortic valve, characteristic of aortic stenosis. Annual echocardiograms helped monitor her condition. When a combination of monitoring and symptoms indicated that the time was ripe for a fix, she underwent a minimally invasive procedure called transaortic valve replacement—and was walking again six hours after surgery.
Kimberly Skelding, MD, FACC, FAHA, FSCAI
“The time is coming when we will be able to, for example, automate echocardiography screening in patients with a heart murmur to detect problems such as aortic stenosis, or a narrowed aortic valve, which can be life threatening,” says Kimberly Skelding, MD, Division Chief of Cardiovascular Services for Jersey City Medical Center and a member of RWJBarnabas Health Medical Group. “Nationally, we are treating less than 30 percent of patients with aortic stenosis who would benefit from a visit with a cardiologist and a discussion about treatment. Cardiac imaging studies hopefully soon will generate a letter—just like we do for mammograms—letting a patient know that they have this diagnosis and should seek care from a cardiologist.”
“We are at the brink of a revolution in cardiac imaging,” says Esad Vucic, MD, PhD, Director of Cardiac Imaging at Newark Beth Israel Medical Center. “The integration of artificial intelligence will vastly enhance our capabilities to detect subtle changes in the heart vasculature and heart muscle. This will allow us much earlier risk prediction for heart attacks or heart failure—an advancement that will greatly benefit our patients.”
Kameswari Maganti, MD, FACC, FASE
“Surveillance of valve diseases at specific stages, for example, allows us to monitor the progression of the disease and its impact on heart function, and allows precise timing of valve intervention so that patients receive the appropriate treatment at the most propitious moment for the best benefit,” says Kameswari Maganti, MD, FACC, FASE.
“Surveillance of valve diseases, for example, allows us to time valve surgery precisely so that the right patient receives the right treatment at the right moment for the right benefit,” says Ajay Shah, MD, a cardiologist with RWJBarnabas Health Medical Group. “RWJBH has enormous resources in both advanced technologies and expertise that—combined with pioneering work in artificial intelligence—will have a huge and growing impact on picking up problems much earlier, which will translate to amazing patient care.”
Learn more about cardiovascular imaging at RWJBarnabas Health.




 View full issues of Healthy Together magazine by New Jersey region:
View full issues of Healthy Together magazine by New Jersey region: