Cardiac Tamponade
Cardiac Tamponade is a cardiac emergency and can be fatal if not diagnosed and treated quickly. Anyone who experiences an acute onset of chest pain or pressure, shortness of breath, irregular heartbeat, and a feeling of drowsiness should call 911 immediately. The acute onset of these symptoms could indicate the early stages of pericardial effusion, cardiac tamponade, or of another cardiac-related condition.
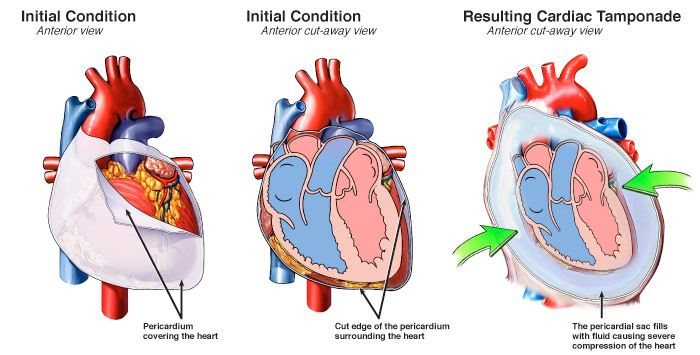
The heart is surrounded by a double-layered sac called the pericardium. Between these two layers, there is a space known as the pericardial cavity. The pericardial cavity normally contains a small amount of pericardial fluid. This fluid prevents friction between the two layers and helps your heart move easier within the sac. If too much fluid accumulates between the pericardium and the heart itself, the condition is known as pericardial effusion.
A normal pericardium can stretch to accommodate increases in pericardial volume, with the stretch amount related to how quickly the effusion develops. Regardless, ongoing accumulation of pericardial fluid into a closed space will eventually lead to an increase of the intra-pericardial pressure. When the intra-pericardial pressure becomes too high, cardiac function becomes impaired and a condition called cardiac tamponade occurs. Cardiac tamponade may develop rapidly (acute) or gradually (chronic). If not treated, cardiac tamponade can lead to cardiac arrest and eventually death.
Medical Illustration Copyright © 2019 Nucleus Medical Media, All rights reserved.
Causes of Cardiac Tamponade
Cardiac tamponade is caused by the increased intra-pericardial pressure that occurs due to the speed and amount of fluid accumulation (pericardial effusion) between the two layers of the pericardium (pericardial cavity).
Other conditions that may contribute to the development of cardiac tamponade:
- Malignancy “cancerous” spread.
- End-Stage Renal Disease: A condition in which your kidneys have stopped working well and your body retains fluid.
- Viral, bacterial, fungal or parasitic infections.
- Idiopathic “no known cause” pericarditis.
- Sharp or blunt chest trauma.
- Thyroid Disease: A condition that is caused by the over or under function of the thyroid gland. The thyroid gland is an essential organ for producing thyroid hormones, which maintains the body’s metabolism.
- Autoimmune Disease: A condition in which your immune system mistakenly attacks your body (e.g. lupus, rheumatoid arthritis and scleroderma).
- Invasive heart/lung surgical procedures.
- Rupture of an aortic aneurysm
Symptoms of Cardiac Tamponade
Common symptoms of cardiac tamponade include:
- Chest pain or pressure
- Shortness of breath
- Heart palpitations
- Lightheadedness/Fainting
- Confused or impaired thinking
- Nausea and/or vomiting
- Decreased urine output
- Anxiety
- Swelling of the legs or abdomen
Diagnosis of Cardiac Tamponade
The clinical diagnosis of cardiac tamponade is usually based on the patient’s medical history and physical examination findings. After that, you may have one or more of the following diagnostic tests and procedures:
Treatment of Cardiac Tamponade
The definitive treatment for cardiac tamponade is removal of the accumulated pericardial fluid. This is performed by employing one of the following procedures:
