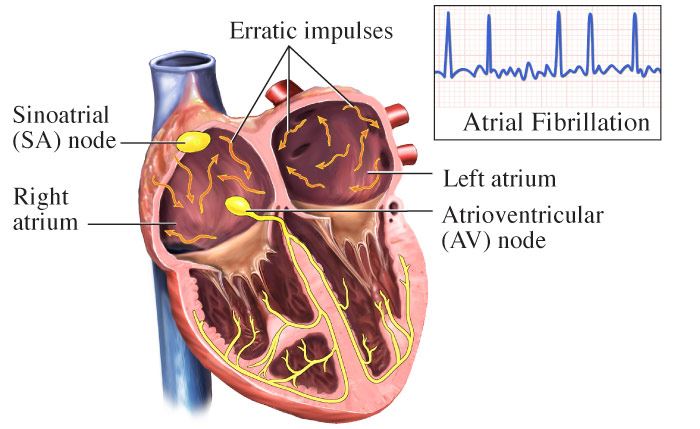
Atrial Fibrillation
The heart beat (contraction) begins when an electrical impulse from the sinoatrial node (SA node) moves through it. The SA node is sometimes referred to as the heart's "natural pacemaker" because it initiates impulses for the heartbeat. These impulses follow a very specific pattern every time; however, this exact route must be followed for the heart to pump properly. As long as the electrical impulse is transmitted normally, the heart pumps and beats at a regular pace. In an adult, a normal heart beats 60 to 100 times a minute.
When the SA node has issues though, you get a change in your heart's rhythm. This is known as an arrhythmia. Almost everyone has felt some type of arrhythmia throughout their life. Some examples include: a “fluttery” feeling in the chest or the feeling of the heart “skipping” a beat. Don’t panic if you’ve occasionally had these symptoms, as most are harmless. However, arrhythmias that last for longer periods of time, may present some problems. One of these is atrial fibrillation (AFib).
Atrial Fibrillation (AFib) is the most common type of arrhythmia. During AFib, control of electrical activity in the atria (heart’s upper chambers) becomes disorganized. This causes the atria to “quiver” or fibrillate. The disorganized signals are then transmitted to the ventricles (heart’s lower chambers) causing them to contract irregularly and sometimes at a much faster pace (about 350-600 beats per minute). The contraction of both heart chambers is no longer coordinated, and the amount of blood pumped out to the body will vary with each heartbeat.
Atrial fibrillation is similar to another type of arrhythmia, atrial flutter (AFL). In AFL, the heart beats abnormally fast, but in a regular pattern. With AFib, the heart beats fast and in no regular pattern or rhythm. Both of these conditions lead to a poor contraction of the atria which leads to blood pooling in the heart and can eventually lead to the formation of blood clots. If the blood clots become loose and travel in the bloodstream, it raises the significant risk for a stroke.
Medical Illustration Copyright © 2019 Nucleus Medical Media, All rights reserved.
Types of Atrial Fibrillation
- Paroxysmal Atrial Fibrillation: This type of atrial fibrillation occurs when your heart goes in and out of normal rhythm for less than a week. You might feel this happening for a few minutes or for several days. Treatment is usually not required. Doctors call this type “holiday heart syndrome.” It happens to otherwise healthy people celebrating with a late night out or having a few extra drinks. It also happens when you’re under extreme stress.
- Persistent Atrial Fibrillation: This type of atrial fibrillation occurs when your heart goes in and out of normal rhythm for longer than a week. This condition may become permanent or it may stop on its own, however it’s possible you could need medicine or treatment to stop it.
- Permanent (Chronic) Atrial Fibrillation: This type of atrial fibrillation cannot be corrected by treatments. If you have this type, you and your doctor will decide on the best plan of action.
Causes of Atrial Fibrillation
Although the exact cause is unknown, certain conditions, traits or habits may raise your risk for the condition. These are known as risk factors.
Non-Modifiable Risk Factors: These factors are irreversible and cannot be changed. The more of these risk factors you have, the greater your chance of developing atrial fibrillation.
- Although it can happen at any age, risk increases with older age.
- Family history/genetics
- Previous heart attack
Modifiable Risk Factors: These factors can be modified, treated or controlled through medications or lifestyle changes.
- High blood pressure
- Diabetes: When your blood glucose, also called blood sugar, is too high.
- Obesity or having a body mass index “BMI” of 30 or greater.
- Excessive alcohol consumption over many years.
- Extreme emotional stress.
- Excessive amounts of caffeine or other stimulants.
- Long history of cigarette smoking and/or drug abuse.
Other conditions that contribute to development of atrial fibrillation:
- Heart surgery
- Heart valve disease
- Heart failure
- Thyroid Disease: A condition that is caused by the over or under function of the thyroid gland (the thyroid gland is an essential organ for producing thyroid hormones, which maintains the body’s metabolism).
- Obstructive Sleep Apnea: A condition in which your breathing abruptly stops and starts while sleeping.
Symptoms of Atrial Fibrillation
Some people with atrial fibrillation have no symptoms. Others are unaware of their condition until it's discovered during a physical examination. Those who do have atrial fibrillation symptoms may experience the following:
- Chest pain, fullness, discomfort or pressure.
- Confused or impaired thinking.
- B.E. F.A.S.T.: balance loss, eye blurriness, face drooping, arm weakness, speech difficulty — time to call 911.
- General fatigue or fatigue when exercising.
- Rapid heart rate (tachycardia) of over 100 beats per minute.
- Heart palpitations
- Lightheadedness/fainting
- Shortness of breath
- Cold sweat
Diagnosis of Atrial Fibrillation
To diagnose atrial fibrillation, your doctor may review your signs and symptoms, your medical history and conduct a physical examination. After that, you may have one or more diagnostic tests and procedures including:
Treatment of Atrial Fibrillation
Treatment depends on the severity of your AFib condition, any other underlying medical issues you might have, and the length of the AFib condition. Based on the findings, your doctor may recommend treatments including lifestyle changes, medications or medical or surgical procedures.
Lifestyle Changes
- Avoid smoking.
- Eat a heart-healthy diet.
- Exercise under directions of your doctor.
- If you're overweight, talk to your doctor about weight loss options.
- Manage stress.
- Limit alcohol consumption and caffeine consumption.
- Make and keep appointments to see your doctor for routine checkups and follow-up tests.
Medications
- Antiarrhythmic medications will help control your heart’s rhythm.
- Anticoagulants “blood-thinners” will help treat, prevent, and reduce blood clotting ability.
- Beta blockers will help reduce your blood pressure.
- Calcium channel blockers will help relax blood vessels and increase the supply of blood and oxygen to the heart while also reducing the heart's workload.
