Peripheral Arterial Disease
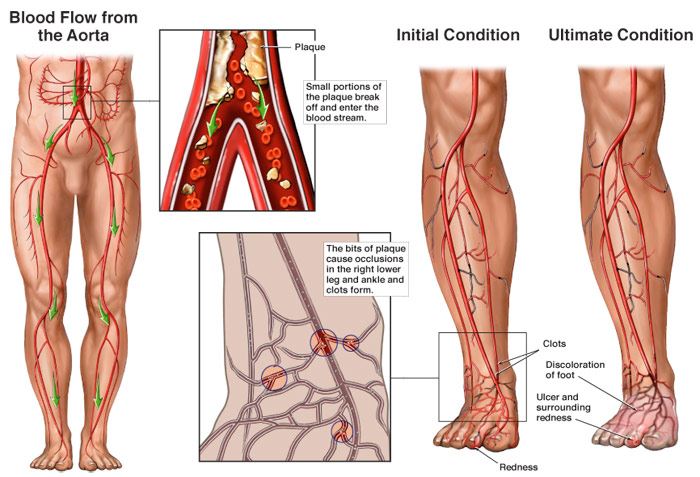
Peripheral Arterial Disease (PAD) is a chronic (gradually developed) circulatory disease in which the arteries supplying blood to your arms and legs become narrowed. The narrowing is due to the buildup of plaque (atherosclerosis) inside the wall of the arteries. As plaque builds up, the walls of these arteries start thickening. This thickening leads to a reduced amount of blood flow to organs and tissues connected to these arteries. If allowed to progress, blood flow in that artery can become limited or blocked all together. If severe enough, people with PAD are at risk of heart attack and stroke.
Medical Illustration Copyright © 2019 Nucleus Medical Media, All rights reserved.
Causes of Peripheral Arterial Disease
The main cause of PAD is atherosclerosis. However, other conditions, traits or habits may raise your risk for the disease. These conditions are known as risk factors and include:
Non-Modifiable Risk Factors: These factors are irreversible and cannot be changed. The more of these risk factors you have, the greater your chance of developing PAD.
- Family history/Genetics
Modifiable Risk Factors: These factors can be modified, treated or controlled through medications or lifestyle changes.
- Long history of cigarette smoking and/or drug abuse.
- High cholesterol
- High blood pressure
- Diabetes: When your blood glucose, also called blood sugar, is too high.
- Obesity or having a body mass index “BMI” of 30 or greater.
Other conditions that contribute to the development of PAD:
- End-Stage Renal Disease: A condition in which your kidneys have stopped working well and your body retains fluid.
Symptoms of Peripheral Arterial Disease
While many people with PAD have mild or no symptoms, some people experience a variety of the following symptoms:
- Fatigue or cramping of your muscles in the calf, thigh, hip or buttock.
- Pain in your toes or feet while resting.
- Coldness in your lower leg or foot, especially when compared with the other side.
- Leg numbness or weakness.
- Open wound or ulcers on your toes or feet.
Diagnosis of Peripheral Arterial Disease
You will be asked questions about symptoms and medical history, including questions about family members. A physical exam will also be performed. After that, your doctor may recommend diagnostic tests. Some of the diagnostic tests and procedures include:
- Ankle-Brachial Index (ABI) test
- Angiogram
- Computed tomography (CT scan)
- Magnetic resonance imaging (MRI)
Treatment of Peripheral Arterial Disease
In most cases, you can manage PAD through a combination of medication and lifestyle changes. This can reduce your symptoms and lower your chances of having a heart attack or stroke. Treatment options include:
Lifestyle Changes
- Avoid smoking.
- Exercise under directions of your doctor.
- Eat a heart-healthy diet.
- If you’re overweight, talk to your doctor about weight-loss options.
- Take care of your feet.
- Make and keep appointments to see your doctor for routine check-ups and follow-up tests.
Medications
- Anticoagulants “blood-thinners” will help treat, prevent, and reduce blood clots.
- Beta blockers will help reduce your blood pressure.
- Blood sugar medications will help regulate your blood glucose levels.
- Statins will help reduce the level of cholesterol in the blood.
