Cardiomyopathy
The heart is a muscle that pumps blood throughout the body. Cardiomyopathy occurs when the muscle in the heart thickens, stiffens, thins, or fills with substances produced by the body that do not belong in the heart muscle. As a result, the heart’s ability to pump blood is reduced, which can lead to arrhythmias, the backup of blood into the lungs or rest of the body, and heart failure.
Types of Cardiomyopathy
-
Dilated Cardiomyopathy (DCM): The most common type of cardiomyopathy. In dilated cardiomyopathy, the
heart’s ability to pump blood is decreased because the left ventricle
(heart’s main pumping chamber) is enlarged, dilated and weak. As
a result, the heart muscle doesn't contract well and cannot pump blood
very effectively. In up to 50 percent of the cases, the illness may have
a hereditary component.
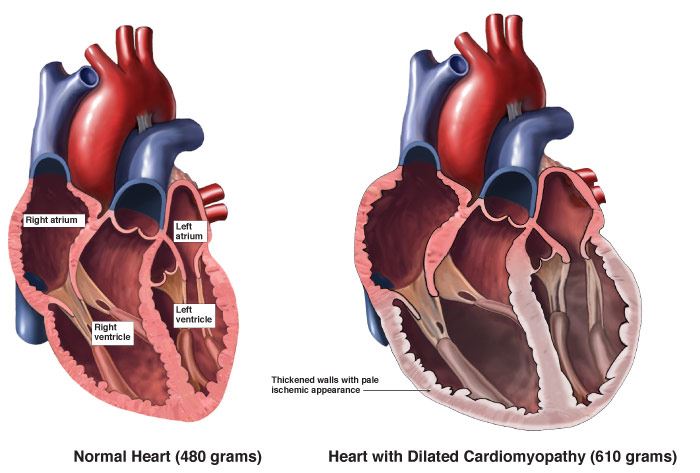
Medical Illustration Copyright © 2019 Nucleus Medical Media, All rights reserved. - Hypertrophic Cardiomyopathy (HCM): This type of cardiomyopathy occurs if the heart muscle cells enlarge, which causes the walls of the ventricles (usually the left ventricle) to thicken. As a result of the thickening, the heart cannot relax well and thus cannot fill with blood. In approximately 50 percent of the cases, a genetic mutation can be found.
-
Arrhythmogenic Right Ventricular Dysplasia (ARVD): A rare type of cardiomyopathy. It occurs when the muscle tissue in the
right ventricle dies and is replaced with fatty or fibrous tissue. This
disrupts the heart’s electrical signals and causes arrhythmias.
ARVD usually affects teens or young adults and can cause
sudden cardiac arrest in young athletes. It is known to be hereditary.
There are other types of cardiomyopathy that do not fit well into the general classifications. - Stress-Induced Cardiomyopathy (Broken Heart Syndrome or Takatsubo Cardiomyopathy): This type of cardiomyopathy usually happens as a result of extreme emotional and physical stress and can cause rapid and severe heart muscle damage. The condition is more common in post-menopausal women.
- Peripartum Cardiomyopathy (PPCM): This type of cardiomyopathy is a rare form of congestive heart failure that is associated with pregnancy. If you have peripartum cardiomyopathy, your heart becomes weak and larger than normal. Most times, PPCM occurs in the last trimester of pregnancy or the first month after delivery, but sometimes it takes up to 6 months after delivery for the condition to occur.
Causes of Cardiomyopathy
Although the exact cause is unknown, certain conditions, traits or habits may raise your risk for the condition. These are known as risk factors and include:
Non-Modifiable Risk Factors: These factors are irreversible and cannot be changed. If you have a family history or genetic predisposition, the greater your chance of developing cardiomyopathy.
Modifiable Risk Factors: These factors can be modified, treated or controlled through medications or lifestyle changes.
- Diabetes: When your blood glucose, also called blood sugar, is too high.
- Long history of cigarette smoking and/or drug abuse.
- Obesity or having a body mass index “BMI” of 30 or greater.
- High blood pressure
- Excessive alcohol consumption over many years.
- Nutritional deficiencies of key vitamins and minerals.
Other conditions that contribute to the development of cardiomyopathy:
- Amyloidosis
- Rapid heart rate (tachycardia) of more than 100 beats per minute.
- Certain infections, especially those that inflame the heart.
- Heart valve disease
- Congenital heart disease
- Coronary artery disease
- Hemochromatosis: A condition in which iron builds-up in your heart muscle.
- HIV
- Thyroid Disease: A condition that is caused by the over or under function of the thyroid gland. The thyroid gland is an essential organ for producing thyroid hormones, which maintains the body’s metabolism.
- Autoimmune Disease: A condition in which your immune system mistakenly attacks your body (e.g., lupus, rheumatoid arthritis and scleroderma).
- Muscular Dystrophy: A group of diseases that progressively cause weakness and loss of muscle mass.
- Obstructive Sleep Apnea: A condition in which your breathing abruptly stops and starts while sleeping.
- Use of some chemotherapy drugs and radiation to treat cancer.
Symptoms of Cardiomyopathy
In the early stages of cardiomyopathy there might be no signs or symptoms. But as the condition advances, signs and symptoms usually appear, including:
- Bloating of the abdomen due to fluid buildup.
- Coughing while lying down.
- Fatigue
- Heart arrhythmias
- Heart palpitations
- Lightheadedness/fainting
- Low blood pressure
- Shortness of breath with exertion or even at rest.
- Swelling of the legs, ankles and feet.
Diagnosis of Cardiomyopathy
Your doctor will conduct a physical examination, take a personal and family medical history, and ask when your symptoms occur. If your doctor thinks you have cardiomyopathy, you might need one or more of the following diagnostic tests and procedures:
- Blood tests
- Cardiac catheterization
- Computed tomography (CT scan)
- Magnetic resonance imaging (MRI)
- X-Rays
- Angiogram
- Echocardiogram (ECHO)
- Electrocardiogram (EKG/ECG)
- Stress test
- Genetic testing
- Biopsy
Treatment of Cardiomyopathy
People who have cardiomyopathy but no signs or symptoms may not need treatment. For others, treatment is needed. Treatment depends on the type of cardiomyopathy, severity of symptoms and complications, your age and overall health. Treatment options include lifestyle changes, medications, and medical and surgical procedures.
Lifestyle Changes
- Avoid alcohol consumption.
- Avoid smoking.
- Eat a heart-healthy diet.
- Enrollment in a cardiac rehabilitation program.
- If you are overweight, talk to your doctor about weight loss options.
- Manage stress.
- Make and keep appointments to see your doctor for routine checkups and follow-up tests.
Medications
- Antiarrhythmic medications will help control your heart’s rhythm.
- Thrombolytic therapy is the administration of drugs called “lytics” or “clot busters” that will help break up or dissolve blood clots.
- Anti-inflammatory medications will help reduce inflammation and relief pain.
- Beta blockers will help reduce your blood pressure.
- Diuretics “water pills” will help reduce the amount of fluid retention in your body.
